CROI 2018 Boston
Earlier this month I attended the 25th CROI in Boston, the conference on retroviruses and opportunistic infections, a wonderful annual opportunity for scientists and clinicians from around the […]
 Dr Fiona Bisshop
Dr Fiona Bisshop
HIV Doctor,Trans Health Advocate, LGBTI Health Provider, Writer for QNews as "Doc Q"
Earlier this month I attended the 25th CROI in Boston, the conference on retroviruses and opportunistic infections, a wonderful annual opportunity for scientists and clinicians from around the […]

Despite my trip beginning and ending with famous Boston “Nor’Easters” which delayed all my flights, covered the eastern US with snow, and at one stage left me stranded in Denver airport wondering if we would need the prolifically sign-posted tornado shelters, I did manage to attend the whole conference; and I was also lucky enough to be invited to a fantastic post-conference meeting with Dr Paul Sax and the faculty from Harvard. The conference covered a large number of topics, with many sessions running concurrently, making it difficult to choose which talks to attend – suffice to say my dance card was always full and sometimes double-booked.
The week began with a self-imposed compulsory running tour of the Boston Freedom Trail, completed in arctic conditions with my new running pal, Dr Laura Waters, sexual health physician from the Mortimer Market Centre in London, our sweet guide, a girl called Ginger, who we decided probably normally runs a half-marathon before breakfast, and some young ladies from LA with very white teeth.

In between freezing to death, we learned all sorts of fascinating historical facts, such as the origin of the term “hooker” to describe General Hooker’s late night lady visitors who used the secret side entrance to the State House, or the fact that all the headstones at the Granary Burying Ground were rearranged in the 19th century into neat rows to make way for the newly invented lawnmower, meaning unwary tourists are at risk of falling into unmarked holes in the ground if they stray off the path whilst taking selfies. Incidentally, I thoroughly recommend the concept of the running tour – I’ve done these a couple of times, and they are an excellent way to get your bearings in a new place, whilst learning interesting stuff, and you get to feel quite superior to everyone else who just went to the hotel buffet breakfast (you can still do the buffet after your run though!). This one was organized by the Freedom Trail Run
So, the conference……as I said it was content heavy. Most of the sessions can be viewed or listened to as webcasts.
I’d like to start by sharing with you an amazing animation by Janet Iwasa from the University of Utah – it represents the HIV replication process, and was showing on a big screen at the conference opening reception. I was transfixed by it.
You can see more of Janet’s work at her website science of HIV
The new single tablet regimen that has been licensed in the US, bictegravir/FTC/TAF (called Biktarvy there – who gets paid to come up with these names?) is looking like a great option – it’s proving to be just as effective at maintaining viral suppression as the other current single tablet options, and it has no booster and virtually no drug interactions. Bictegravir also seems to have a higher barrier to resistance than dolutegravir, and has maintained suppression even in people whose virus has integrase inhibitor resistance mutations, with data now out to 72 weeks. It also looks like people whose virus has archived resistance to NRTIs (even M184V) will also remain suppressed on this treatment. Importantly, the TAF component of the pill also suppresses Hepatitis B very well, so it will be a suitable option for people co-infected with Hep B and HIV. Given the Hep B effect with TAF, it would be very important to avoid sudden cessation of treatment in co-infected patients to avoid a Hep B flare.
There was a study presented showing that switching from dolutegravir/abacavir/3TC to bictegravir/FTC/TAF resulted in continued viral suppression, with fewer side effects and no emergence of resistance. The bictegravir STR is expected to be licensed in Australia in the near future.
There’s a new kid on the block – MK8591 (also called EFdA) – it really does need a snappier name, but I think we will be hearing more about this one in the future. It’s from a new class of antiretrovirals, nucleoside reverse transcriptase translocation inhibitors (NRTTIs), has a very long half-life in the body, and is highly potent. It’s being studied for its suitability as both a treatment (combined with doravirine) and as PrEP, possibly as either a weekly pill or as an implant.
Another completely new drug in a new class is Ibalizumab. It’s a monoclonal antibody, given as an intravenous infusion every 2 weeks. It’s active against multi-resistant HIV, and has been approved in the US for people with very limited treatment options due to resistance. It prevents HIV from entering T cells by binding to their CD4 receptor. It’s the first new drug option we’ve had for salvage therapy in quite a while.
Broadly neutralizing antibodies (BNAbs) are another form of immunotherapy that may get traction in the future. They have promising potential for use in both prevention and treatment, as they target the HIV envelope protein. They are likely to be quite expensive to manufacture however, and their long-term safety and efficacy is unknown.
As we all know, there is still no cure for HIV. The only person ever to have been cured of HIV is the “Berlin” patient, Timothy Ray Brown, who effectively received a complete immune system transplant as treatment for acute myeloid leukaemia. He was transplanted with stem cells from a donor who was resistant to HIV infection due to a mutation (CCR-5 delta 32 deletion if you want to get technical) which stops the virus from being able to attach to and enter T cells in the first place. You can read an interview with him here
In everybody else, HIV persists despite long-term treatment. If treatment is stopped, viral rebound (ie measurable virus in the blood again) occurs after 3 to 4 weeks. In people who started their treatment very early after contracting HIV, the time to rebound is longer, but it still happens. It’s because there is a reservoir of HIV in parts of the body that is not able to be reached by current treatments. A crucial site is in the lymph node B cell follicles. These guys might as well hang a shingle out that says “HIV lives here, not at home to visitors”.
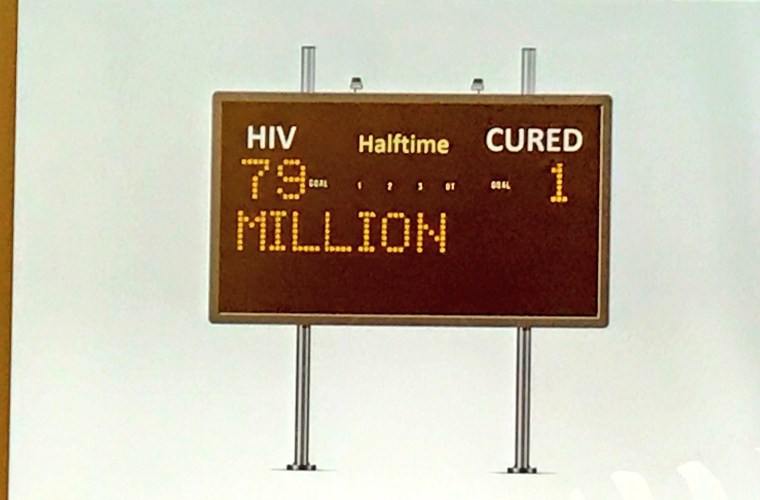
As Jonathan Li from Harvard Medical School pointed out, at this point in the game, the scoreboard is not promising, but there may be great things to come.
So where is cure research heading?
It’s not more bone marrow transplants – there have been several attempts to replicate what happened in the Berlin patient, but so far these have been flatly unsuccessful – the longest anyone took to rebound was 8 weeks.
It’s not adding more antiretrovirals – studies adding the integrase inhibitor dolutegravir to a successful 3 drug regimen have not resulted in a cure.
There are 2 areas of cure research that are looking promising. The first is the “shock and kill” approach, which tries to get HIV out of its hiding places into the open, then destroying it. A combination of a TLR7 agonist then a BNAb has been tested in monkeys who were treated early with ART, and half of the monkeys became post-treatment controllers (maintaining viral suppression off any treatment), and even more impressively their blood and lymph nodes were not infectious! (I have to confess that I am not at all comfortable with the use of monkeys in medical research, however I do understand that live models are the only way to test these treatments).
The 2nd area is gene therapy, using zinc finger nucleases to induce breaks in the CCR5 gene. I can’t get more technical than this about it without my brain exploding, sorry. This could well be a future cure, though so watch this space!
In the words of Antony Fauci from the NIH,
However, HIV presents unique challenges to vaccine scientists. Its extensive viral clade and sequence diversity, the establishment of latent reservoirs and its evasion of the cellular and humoral immune responses all make it extremely difficult to make an effective vaccine.
It’s not safe to use an attenuated virus as a vaccine (which is what we do for measles and chickenpox), and there is no small animal model that replicates human HIV infection, so vaccine testing is very expensive (damn those expensive monkeys), and there has been relatively little interest from pharmaceutical companies up until now.
A vaccine needs to be more than 50% protective to be of any public health benefit. Only 4 vaccines have ever made it to clinical trials, and only one showed any clinical benefit – the Thai trial in 2009 – and this showed only 31% protection.

Now a new multivalent mosaic vaccine is entering phase 2b clinical trials after showing a 100% antibody response in recipients. The trial is enrolling women in Africa and is called Imbokodo, which means rock in Zulu, referring to the strength of women. Findings are due in 3 to 4 years, and I am truly excited about this one!
These days PrEP (Pre-exposure prophylaxis for HIV) is getting almost as much attention as treatment at HIV conferences, and with good reason – it works!
Speakers from Sydney and San Francisco both described how the introduction of PrEP in their respective cities has led to a striking drop in new diagnoses. In NSW the drop was 35% according to Andrew Grulich from the Kirby Insititute.
PrEP failures – despite the many thousands of people on PrEP all over the world, there have only been 4 reported cases of PrEP failure, and in at least 2 of these the cause was resistant virus, ie these unlucky individuals were infected with a virus which was already resistant to the drugs in PrEP. The likelihood of this occurring is very low, as resistant virus is fairly rare. The most recent PrEP failure appears to be due to poor clinical oversight and intermittent adherence – the individual involved was given a 12 month supply of medication, and had a seroconversion during that period. Hair tenofovir levels showed they were adherent at the time of diagnosis at least, and their virus has resistance, although it is not clear if it was pre-existing or developed due to exposure to PrEP after infection.
There was a very interesting presentation by Julia Schillinger on the relationship between PrEP and the increase in sexually transmitted infections (STIs). There is much concern that PrEP is driving up the rate of syphilis, gonorrhoea and chlamydia, but it’s not as simple as that. People are being tested more often and at more bodily sites, and there is increased availability of rapid tests and self-collection of swabs. While PrEP drives increased testing, it also leads to increased treatment which prevents onwards transmission. Condomless sex is certainly increasing, but the increase in STIs started well before the widespread availability of PrEP, in fact pretty much since the advent of smart phones!

Should we blame meet-up apps? Statistical modelling suggests that if 40% of the at-risk population were to be on PrEP, the rates of STIs would actually fall by 40%. I’m not sure exactly how that works, but would love it to be true!
The president of the International AIDS Society, Linda-Gail Bekker dispelled some myths regarding PrEP:
For PrEP to truly have an impact on HIV transmission across the globe, it needs to be accessible to all high risk populations, including people who inject drugs, women, people from high prevalence countries and their partners.
We know that HIV infection raises the risk of heart disease, but what can we do about it? In fact, the most profound intervention for risk reduction is stopping smoking, but unfortunately this is the hardest to implement. So what else can we do? Using statins to lower cholesterol and treating high blood pressure are important interventions, but another risk-reducing step is to consider switching off abacavir (ABC) therapy.
ABC has been used in the treatment of HIV for many years, but has been embroiled in controversy regarding its cardiovascular risk ever since the D:A:D study findings were reported at CROI 10 years ago. We are now finally getting a better understanding of how it influences cardiovascular risk. It causes more reactive platelets, making them sticky. The increased risk appears to climb over the first 6 months of ABC use, and then level off. Aspirin cannot counteract this effect as it acts via a different pathway. A Swiss study has shown that when patients are switched from ABC/3TC to TAF/FTC, there is an on/off effect whereby platelet aggregation immediately decreases. This study did not measure any cardiovascular events, however what has been shown is that ABC is associated with a 50% increased risk of non-calcified plaque in the coronary arteries. This unstable plaque is more likely to rupture and accounts for 75% of myocardial infarcts. It won’t show up on a coronary calcium CT.
Cardiologist Professor Priscilla Hsue from UCSF has a list of the most useful interventions in reducing cardiovascular risk in HIV+ patients, in order of their effectiveness.
(Note that smoking should of course be discussed whenever possible, but it’s at the bottom because it’s the hardest change to achieve).
There are many reasons why someone might be on an ABC-based regimen, so simply switching off it may not be a sensible option, however in people with other risk factors for heart disease it should be considered.
Incidentally there was some very interesting data presented on rates of cancers in statin users, based on an analysis of the US Veterans Aging Cohort Study. Apart from having lower cholesterol, people on statins have an overall 40% reduction in cancers, and the benefit increased to 49% in HIV + people. The protective effect was strongest for virus-related cancers. Non-Hodgkin’s lymphoma dropped by 71%, oral cancer by 65%, lung cancer by 51% and anal cancer by 38%, and all-cause mortality dropped by 45%. Watch out for the REPRIEVE study (currently enrolling), which is evaluating the statin effect on heart disease in HIV, and will also look at cancer incidence.
It snowed a few times while I was in Boston. Basically every time I tried to go out…..

This is an area where there is a sad lack of data, especially in Australia.
Tonia Poteat, a long-time AIDS activist and epidemiologist from Johns Hopkins University, presented information on HIV in the trans population in the USA, where the HIV prevalence is a shocking 20%. Retention in care is a major challenge.

She also presented on PrEP uptake in this group, and identified transgender women’s fear of PrEP interacting with hormones as a key driver. Healthcare providers can make a difference in this space with some simple education – there is no interaction between oestradiol and TDF/FTC, so we can reassure our trans patients that their hormone levels will not be affected by PrEP.


There was a lot on the vaginal microbiome, which probably deserves its own separate blog. The human microbiome comprises up to 100 trillion organisms which reside in the body, generally without causing harm. There are almost 5kg of bacteria in the gut alone!
Nichole Klatt from the University of Washington presented a plenary session on vaginal dysbiosis, a situation where the normal predominance in the female genital tract of Lactobacillus (the “good” bacteria) is replaced by anaerobic bacteria (such as Gardnerella, but there are many others). The most well-known clinical presentation is bacterial vaginosis. This change in bacterial populations leads to increased inflammation, reducing the integrity of the epithelial barrier, and increasing the likelihood of HIV acquisition. The vaginal microbiome is diverse across different ethnicities, and dysbiosis is more common in African women.
Gardnerella bacteria enhance the degradation of tenofovir (TFV) and dapivirine, and decrease plasma levels of TFV, which would help explain why in the CAPRISA trial which looked at TFV gel as PrEP the efficacy was vastly reduced in women with Gardnerella dominance compared with those with Lactobacillus dominance (18% vs 61%). The implications for the utility of the dapivirine vaginal ring for PrEP are obvious. What I found most interesting was that these dysbiotic bacteria do not degrade TAF (tenofovir alafenamide, the upgrade for TFV), so will we see future TAF-based delivery systems for PrEP?
The big question in everyone’s mind is that now we are spreading the message of U=U (you can’t infect a partner with HIV if you are undetectable), does this apply to breastfeeding mothers who are undetectable?
We still don’t have the answer to that question, and neither do we know the full effects of infant exposure to antiretrovirals through breast milk.
Certainly in developing nations where access to safe drinking water is limited, breastfeeding is safer for the infant overall. We also know that mixed feeding (both breast and bottle) increases the risk of transmission, probably through increased intestinal permeability.
But what about in situations where formula feeding is a safe and affordable option and the mother is suppressed on treatment? Is there any place for breastfeeding? Here are the issues as I see them:
There were so many other interesting presentations and posters, most of which are available to download or watch at the conference website.
Well done if you’ve made it to the end of this long read. I shall reward you with a video of a squirrel on Boston Common after a snowstorm.
Reblogged this on Edie115 and commented:
Reblog from Dr Fiona Bisshop.
CROI 2018. All the goings on in the HIV world.
LikeLiked by 1 person
Nice interesting post.
BY FOR NOW
LikeLike